Tarsal
Tunnel Syndrome
- Home
- Conditions We Treat
- Foot & Ankle
- Tarsal Tunnel Syndrome
What is
tarsal Tunnel Syndrome
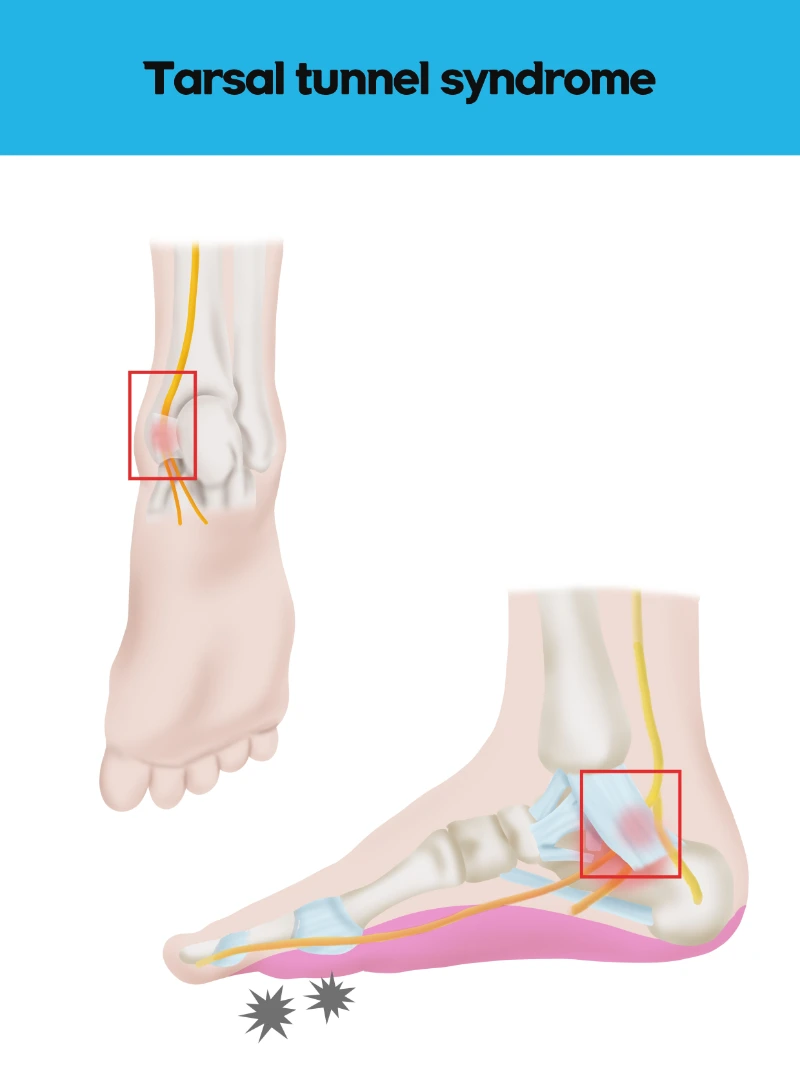
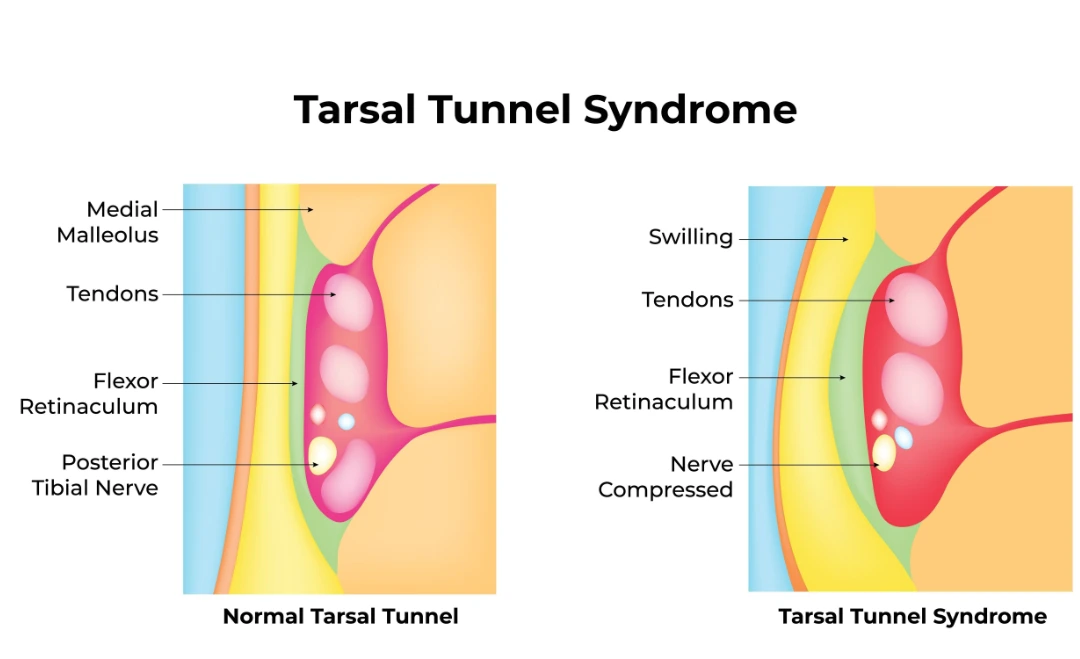
Tarsal Tunnel Syndrome (TTS) is a condition caused by the compression or entrapment of the posterior tibial nerve as it passes through a narrow space called the tarsal tunnel, located on the inside of the ankle. This tunnel is formed by the ankle bones and a dense band of ligaments, through which vital nerves, blood vessels, and tendons pass, which enables movement and sensation in the foot.
When the tibial nerve becomes compressed within the tarsal tunnel, it can lead to a range of symptoms, often described as nerve pain, including burning, tingling, or numbness in the sole or heel of the foot. In some cases, individuals may experience shooting pain or weakness in the foot muscles, which can worsen with physical activity or prolonged standing.
TTS is similar to carpal tunnel syndrome in the wrist, but it affects the foot and ankle. This condition can be caused by several factors, including flat feet, which can stretch the tibial nerve, or conditions that increase swelling in the area, such as arthritis, diabetes, or even ankle injuries. Early diagnosis and treatment are crucial to prevent long-term nerve damage and alleviate symptoms.
What causes tarsal tunnel syndrome?
Tarsal Tunnel Syndrome occurs when the posterior tibial nerve is compressed as it travels through the tarsal tunnel, a narrow passageway located on the inside of the ankle. The tarsal tunnel is formed by the ankle bones and a thick ligament called the flexor retinaculum, which holds and protects various structures passing through the tunnel, including tendons, arteries, veins, and the tibial nerve. Compression of this nerve can occur due to intrinsic or extrinsic factors that create pressure within the tunnel.
Intrinsic factors include abnormalities within the tarsal tunnel itself, such as the presence of ganglion cysts, varicose veins, or scar tissue, which physically narrow the tunnel and impinge on the nerve.
Additionally, inflammation of the surrounding tendons or soft tissues, as seen in conditions like tenosynovitis, can lead to increased pressure within the tunnel. Similarly, perineural fibrosis or the formation of scar tissue around the nerve can further restrict its movement and compress it.
Extrinsic factors, such as trauma or anatomical deformities like a valgus hindfoot, can also play a role. For instance, a severe ankle sprain may lead to swelling and inflammation, which can reduce the available space within the tarsal tunnel and press against the nerve. Systemic conditions like edema, where excess fluid accumulates in the lower extremities, can further increase compression within this narrow space. This compression disrupts the normal functioning of the tibial nerve, leading to the hallmark symptoms of TTS, including pain, numbness, and tingling.

What are the symptoms of tarsal tunnel syndrome?
Tarsal Tunnel Syndrome manifests as nerve pain caused by the compression of the posterior tibial nerve. Symptoms may vary in intensity and location but are generally centred around the foot and ankle. Common symptoms include:
- Burning or tingling sensations in the sole or heel of the foot
- Numbness in the affected area, often radiating to the toes
- Sharp, shooting pain that may worsen with activity or prolonged standing
- Swelling or inflammation in the ankle, contributing to discomfort
- Muscle weakness in the foot, potentially affecting mobility
These symptoms are often aggravated by physical activity or standing for extended periods, and in severe cases, they may persist even during rest.
Who is at risk of tarsal tunnel syndrome in Singapore?
In Singapore, individuals who are at higher risk of developing Tarsal Tunnel Syndrome (TTS) include those whose activities or conditions increase pressure on the tibial nerve within the tarsal tunnel. Some key groups at risk include:
- People with flat feet: individuals with flat feet or fallen arches are more likely to experience overpronation, which places added pressure on the tibial nerve, and increases the risk of compression.
- Athletes: runners, hikers, and other athletes who engage in repetitive foot movements or prolonged weight-bearing activities are at increased risk due to overuse and repeated strain on the tibial nerve.
- People with prior ankle injuries: individuals who have had ankle sprains or fractures may develop scar tissue or swelling, narrowing the tarsal tunnel and compressing the nerve.
- Patients with chronic conditions: conditions like diabetes, arthritis, or oedema that cause swelling in the lower extremities can increase pressure in the tarsal tunnel, leading to nerve compression.
- People with occupational strain: jobs requiring prolonged standing, walking, or wearing non-supportive footwear can elevate the risk of nerve compression in the tarsal tunnel.
In Singapore, where a significant portion of the population leads an active lifestyle and individuals face common chronic conditions such as diabetes, many may fall into one or more of these risk categories. Early diagnosis and preventive measures can help manage and reduce the likelihood of developing TTS.
How is tarsal tunnel syndrome diagnosed?
At Cove Orthopaedic, we take a comprehensive approach to diagnosing Tarsal Tunnel Syndrome. Identifying the exact cause of nerve compression is crucial for developing the right treatment plan. To do this, we use a combination of clinical evaluations and advanced diagnostic tools. Here’s how we proceed with the diagnosis:
- Clinical examination and medical history: we start by thoroughly discussing your symptoms, such as pain, tingling, or numbness in your foot or ankle. Our specialists will ask about any past injuries or conditions that could contribute to nerve compression.
- Tinel’s sign test: this simple, non-invasive test involves tapping over the tibial nerve along the inside of your ankle. If tapping reproduces the tingling or pain you’re experiencing, it helps confirm the presence of nerve compression.
- Imaging Tests (X-rays, MRI, CT scan): if further investigation is required, we may recommend imaging tests to get a detailed look at the structures in and around the tarsal tunnel. X-rays can help identify bone spurs or fractures, while an MRI or CT scan provides a clearer view of soft tissues, such as tendons, cysts, or swollen structures that may be compressing the nerve.
- Electromyography (EMG) and Nerve Conduction Study (NCS): to assess the extent of nerve damage, we may conduct EMG or NCS tests. These tests measure how well the tibial nerve is functioning by checking the electrical activity in your muscles. It helps us pinpoint the severity and location of the nerve compression.
This detailed and personalised diagnostic process ensures that we understand the root of your symptoms and can provide you with the most effective treatment plan.
What are the treatment options for tarsal tunnel syndrome in Singapore?
At Cove Orthopaedic, we tailor treatment for Tarsal Tunnel Syndrome based on the severity of your symptoms and how much the nerve compression has affected your daily activities. Our approach ranges from conservative management to surgical intervention, which helps us ensure that you receive the care that best suits your needs. Here’s how we address this condition:
- Rest and activity modification: the first step in managing TTS is often simply giving your foot time to heal. We may advise resting and avoiding activities that exacerbate your symptoms. Limiting weight-bearing activities can help reduce nerve pressure and promote healing.
- Anti-inflammatory medications: to reduce pain and swelling, we recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen. These medications can help manage discomfort and inflammation around the tibial nerve.
- Custom orthotics or braces: for patients with structural issues, such as flat feet, we offer custom orthotic devices designed to support your foot’s arch. Orthotics help distribute pressure more evenly, reducing strain on the tibial nerve. Braces or splints may also be used to stabilise the foot and limit movements that aggravate the nerve.
- Physical therapy: we may recommend our patients to consult experienced physical therapists, who can create personalised exercise programs to strengthen the muscles in your foot and improve flexibility. Physical therapy can enhance the range of motion and reduce the pressure on the tibial nerves.
- Steroid injections: in cases with inflammation, we may suggest steroid injections to directly target the inflamed tissues around the tarsal tunnel. This can provide temporary relief from pain and swelling and allow the nerve to recover.
- Surgical intervention (Tarsal Tunnel Release): in cases where non-surgical treatments don’t provide adequate relief, we may recommend tarsal tunnel release surgery. This procedure involves relieving the pressure on the tibial nerve by enlarging the tunnel or removing any growths that are compressing the nerve.
Each treatment option is discussed thoroughly with you, and we tailor the approach based on your lifestyle and recovery goals. If you’ve been experiencing symptoms like foot pain, tingling, or numbness, don’t wait for them to worsen. Schedule an appointment with Cove Orthopaedic to get a comprehensive evaluation.
Frequently asked questions
Can Tarsal Tunnel Syndrome go away on its own?
Tarsal Tunnel Syndrome rarely resolves without treatment. The symptoms may worsen over time without proper management. It’s important to consult a healthcare professional early to explore non-surgical treatments that can help alleviate discomfort.
How long does recovery take after Tarsal Tunnel Syndrome surgery?
Recovery after surgery can vary depending on the individual, but most patients use crutches for up to three weeks and experience gradual improvement over a few months. Physical therapy is often recommended to aid in recovery.
Is physical therapy necessary for Tarsal Tunnel Syndrome?
Physical therapy can be beneficial for strengthening foot muscles and improving flexibility, reducing the pressure on the tibial nerve. However, it is not mandatory for every patient, and the need for therapy depends on the severity of your condition.
Can I drive after Tarsal Tunnel Syndrome surgery?
For those who had surgery on their right foot, driving may need to be delayed for a few weeks to ensure safe movement of the ankle. If the surgery was on the left foot, driving may be possible sooner. Always consult your doctor before resuming driving.
Can Tarsal Tunnel Syndrome be prevented?
While there’s no guaranteed way to prevent Tarsal Tunnel Syndrome, wearing supportive shoes, avoiding overuse of the foot, and managing chronic conditions like diabetes can lower your risk.










