Hip
Bursitis
- Home
- Conditions We Treat
- Hip
- Hip Bursitis
Hip bursitis is a painful condition that can make simple movements like walking, climbing stairs, or lying on your side difficult. It occurs when the bursae, small fluid-filled sacs that cushion the hip joint, become inflamed. The result is a deep, aching pain around the outer hip that can limit mobility and affect daily life. Left untreated, it may worsen over time and interfere with even basic activities.

What is hip bursitis?
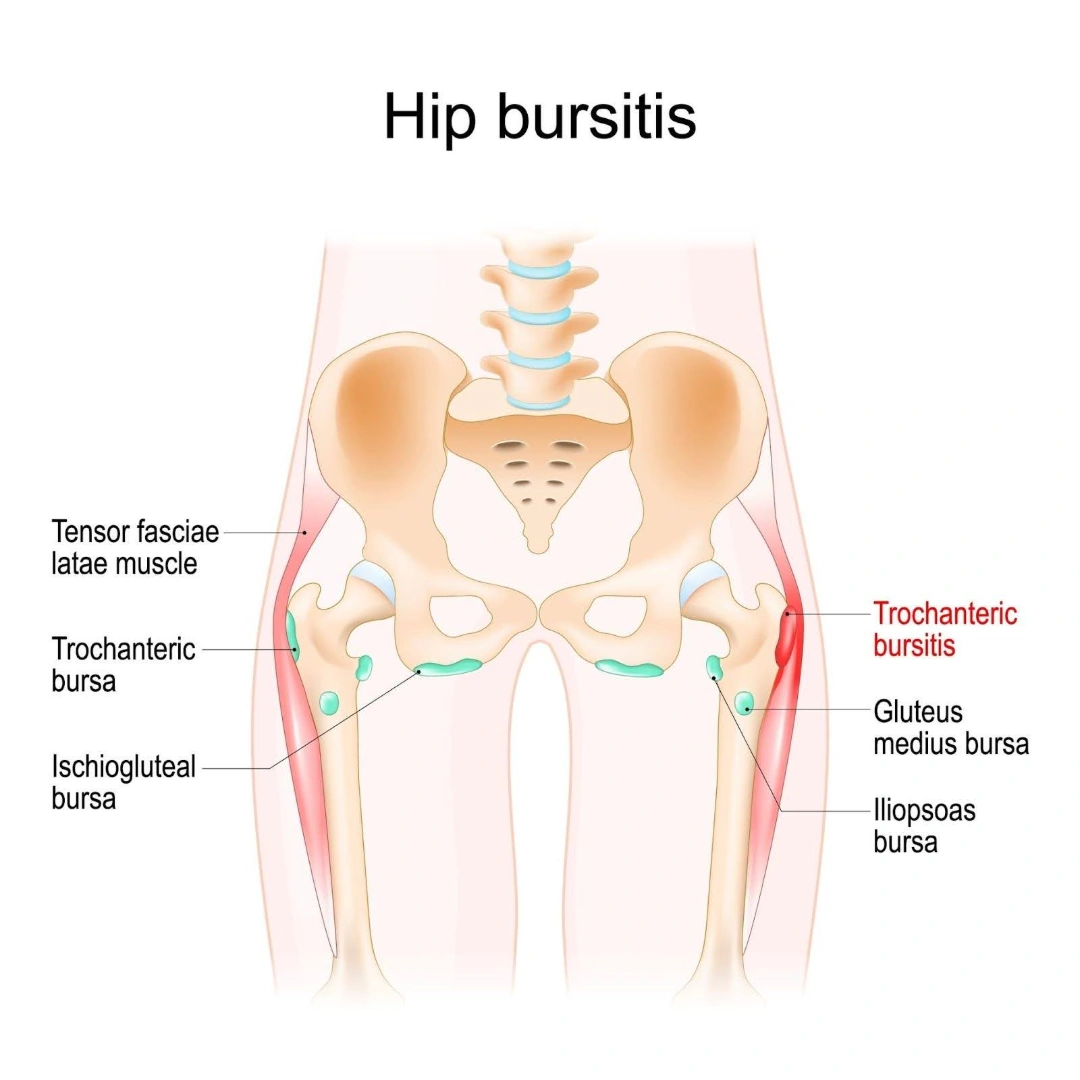
Hip bursitis refers to the inflammation of one or more bursae located around the hip joint. Bursae are small, fluid-filled sacs that act as cushions between bones and soft tissues such as muscles, tendons, and skin. Their main role is to reduce friction and allow smooth, pain-free movement of the joint.
There are two major bursae in the hip that are commonly affected: the trochanteric bursa, located on the outer point of the hip, and the iliopsoas bursa, found on the inner side near the groin. Trochanteric bursitis is the most frequent form and is typically associated with pain over the outer hip and thigh, especially when lying on the affected side, walking, or climbing stairs.
Hip bursitis is not caused by infection but usually results from repetitive motion, direct trauma, joint stress, or underlying conditions such as arthritis or spinal abnormalities. The inflammation can lead to swelling, tenderness, and a dull, persistent ache that may radiate along the thigh. While not typically a serious condition, untreated bursitis can lead to chronic discomfort and impact daily function.
What causes hip bursitis?
Hip bursitis develops when the bursae, small, fluid-filled sacs that cushion the hip joint, become inflamed due to repeated friction, pressure, or trauma. This inflammation often results from physical strain or structural issues that irritate the bursa over time. Common causes of hip bursitis include:
- Repetitive motion — activities such as running, stair climbing, or prolonged standing can overload the hip joint, leading to bursal irritation.
- Direct injury — a fall or impact on the outer hip can bruise the bursa and cause acute inflammation.
- Muscle tightness or imbalance — uneven tension from surrounding muscles or tendons can place extra stress on the bursa.
- Underlying joint conditions — disorders like osteoarthritis, rheumatoid arthritis, or tendinopathy may inflame nearby bursae.
- Previous hip surgery — past surgical procedures or hip implants can alter joint alignment and increase pressure on the bursa.
- Bone spurs — bony overgrowths on the hip can rub against the bursa and cause chronic inflammation.
In most cases, hip bursitis results from a combination of mechanical irritation and joint stress over time, rather than a single event.

What are the symptoms of hip bursitis?
Hip bursitis typically causes discomfort that starts off mild and gradually worsens, particularly with movement or pressure on the affected area. The symptoms may vary depending on whether the inflammation is acute or chronic, but certain signs are commonly experienced.
- Outer hip pain — a dull, aching pain over the outside of the hip, often centred around the bony point (greater trochanter).
- Pain that worsens with activity — movements like walking, climbing stairs, standing up from a chair, or exercising can aggravate the pain.
- Tenderness to touch — the outer hip area may feel sore or tender when pressed.
- Pain when lying on the affected side — many people find it difficult to sleep on the side with bursitis due to direct pressure on the inflamed bursa.
- Swelling or warmth — in some cases, the area may appear slightly swollen or feel warm to the touch.
- Radiating discomfort — pain can sometimes extend down the outside of the thigh but usually does not go past the knee.
If left untreated, these symptoms may become persistent and interfere with sleep, movement, and overall quality of life.
Who is at risk of hip bursitis in Singapore?
Hip bursitis can affect anyone, but certain groups in Singapore may be more prone to developing it due to how they move, age, or underlying medical issues. Recognising these risk groups can help with early intervention and prevention.
- Older adults — as we age, joint wear and tear reduce tissue resilience; this makes bursae more vulnerable to inflammation.
- People with repetitive hip use — those whose hobbies or occupations involve climbing, running, gardening, or other repeated hip movements often overload the joint.
- History of hip injury or surgery — falls, direct blows, previous hip surgery or implants can disrupt joint mechanics and inflame the bursae.
- Spinal or postural conditions — issues like scoliosis or poor posture create uneven pressure on the hips and increase bursitis risk.
- Existing inflammatory or joint diseases — conditions such as rheumatoid arthritis, gout, psoriasis or osteoarthritis may contribute to bursal irritation.
- Occupational or lifestyle factors — manual workers, athletes, and individuals with leg-length discrepancies face higher stress on hip bursae.
- Gender — women are more likely to develop hip bursitis due to differences in biomechanics, including the size, shape, and orientation of the pelvis.
In Singapore, hip bursitis most commonly affects older adults and individuals engaged in physically demanding or repetitive activities, especially when these are combined with past injuries or joint-related conditions.
How is hip bursitis diagnosed?
The diagnosis of hip bursitis is based on a combination of clinical evaluation and, when necessary, imaging tests. A clear understanding of your symptoms, medical history, and physical findings allows the doctor to distinguish bursitis from other causes of hip pain, such as arthritis or tendon injuries.
- Medical history — your doctor will ask detailed questions about the onset, location, and pattern of your pain, as well as any history of trauma, overuse, or underlying joint conditions.
- Physical examination — specific areas of the hip will be gently pressed to check for localised tenderness over the bursa. The doctor may also assess joint movement, gait, and muscle strength to exclude other diagnoses.
- X-rays — while bursae are not visible on X-ray, this test helps rule out other structural problems like fractures or degenerative joint disease.
- Ultrasound — this imaging technique is useful for visualising soft tissue inflammation and fluid accumulation within the bursa.
- MRI — if symptoms persist or the diagnosis is unclear, an MRI may be used to obtain a more detailed view of the hip’s soft tissues.
- Blood tests or bursal fluid aspiration — in rare cases, these may be performed to check for infection or systemic inflammatory disorders.
This diagnostic process ensures that treatment is accurately targeted and complications are avoided.
What are the treatment options for hip bursitis in Singapore?
Managing hip bursitis usually starts with simple, non-invasive measures and progresses to more advanced treatments if needed. The goal is to reduce inflammation, relieve pain, and restore function without compromising daily activity.
Lifestyle measures and self-care — Primary approach for symptom relief
These are the initial steps recommended for most individuals diagnosed with hip bursitis.
- Rest and activity modification — avoid repetitive or aggravating movements such as stair climbing, running, or prolonged standing to allow the bursa to settle.
- Ice therapy — applying a cold pack to the painful area for 15–20 minutes, several times a day, helps reduce inflammation and ease pain.
- Postural adjustments — avoiding positions that put direct pressure on the affected hip, such as sleeping on the painful side, can prevent further irritation.
Medications — To reduce pain and inflammation
Anti-inflammatory medication is often prescribed to manage discomfort.
- NSAIDs — common options include ibuprofen and naproxen, which help relieve both pain and inflammation. These may be taken short-term or as advised by a doctor.
- Topical anti-inflammatory gels — these can be applied directly to the affected area for localised relief with minimal systemic side effects.
Injections — For targeted and longer-lasting relief
When conservative measures are insufficient, injections may be recommended to calm the inflamed bursa.
- Corticosteroid injections — a single injection of steroid medication into the bursa can significantly reduce inflammation and provide relief for weeks or months.
- Ultrasound-guided injections — ultrasound-guided injections help treat hip bursitis by accurately delivering anti-inflammatory medication directly to the inflamed bursa for targeted relief.
Physiotherapy — To restore mobility and prevent recurrence
Physiotherapy plays a vital role in long-term recovery and prevention.
- Stretching and strengthening — targeted exercises help improve hip flexibility and strengthen surrounding muscles to reduce joint strain.
- Manual therapy — hands-on techniques may be used to relieve muscle tension and improve joint alignment.
- Gait and posture correction — addressing abnormal movement patterns or postural habits can prevent the condition from recurring.
- Education and home exercise — patients are guided on safe ways to return to activity and maintain progress at home.
Shockwave therapy — A non-invasive option for persistent cases
Shockwave therapy, or extracorporeal shockwave therapy (ESWT), is increasingly used in Singapore for managing chronic hip bursitis that doesn’t respond to basic physiotherapy or medications.
- Targeted acoustic waves — high-energy sound waves are applied to the affected area to stimulate blood flow, promote tissue healing, and reduce inflammation.
- Outpatient procedure — treatment is done in-clinic, usually once a week for several sessions, with minimal downtime.
Surgical treatment — Rarely required and considered a last resort
Surgery is only advised when all non-surgical approaches have failed and pain continues to interfere with daily life.
- Bursectomy — the inflamed bursa is surgically removed, usually through a minimally invasive procedure. Recovery is generally good, especially when followed by physiotherapy.
- Correction of underlying issues — if bursitis is caused by structural problems, such as bone spurs or abnormal gait, surgical correction may be performed to prevent recurrence.
Most patients experience full recovery with conservative care and proper physiotherapy, and there is rarely a need for invasive intervention.

Summary
Hip bursitis is a common yet often overlooked cause of persistent hip pain that can interfere with walking, sleep, and daily activities. It occurs when the bursae, fluid-filled sacs that cushion the hip joint, become inflamed due to repetitive movement, direct trauma, or underlying joint conditions. Symptoms typically include aching pain over the outer hip, tenderness to touch, and discomfort that worsens with activity or lying on the affected side.
Diagnosis is usually based on clinical assessment, supported by imaging if necessary, to rule out other causes. Most cases respond well to conservative treatment, including rest, physiotherapy, medications, and in some cases, shockwave therapy or corticosteroid injections. Surgery is rarely required.
If you are experiencing ongoing hip pain or discomfort that affects your mobility, schedule a consultation with us for an accurate diagnosis and a personalised treatment plan tailored to your needs.
Conditions We Treat





Frequently asked questions
Can hip bursitis heal on its own?
Mild cases of hip bursitis can improve with rest and activity modification, but persistent symptoms may need medical treatment to avoid chronic pain.
Is hip bursitis linked to sleeping position?
Yes, sleeping on the affected side can worsen hip bursitis symptoms by increasing pressure on the inflamed bursa.
Can sitting for long hours make hip bursitis worse?
Prolonged sitting, especially on hard surfaces, can aggravate hip bursitis by putting continuous pressure on the hip area.
Does hip bursitis affect both hips at the same time?
While it usually affects one side, hip bursitis can occasionally occur on both sides, especially in people with underlying joint issues or repetitive strain.
Can hip bursitis cause pain down the leg?
Yes, the pain can radiate from the outer hip down the outer thigh, but it typically doesn’t go below the knee.
Is walking recommended if I have hip bursitis?
Gentle walking may help maintain mobility, but overdoing it or walking on uneven surfaces can aggravate symptoms. Listen to your body and rest when needed.
Can massage help relieve hip bursitis pain?
Light massage around the surrounding muscles, not directly over the inflamed bursa, may help reduce tension and improve comfort.
How long does hip bursitis take to improve with treatment?
With proper treatment, most people see improvement within a few weeks. Chronic cases may take longer and require physiotherapy or injections.
Can I exercise with hip bursitis?
Low-impact exercises like swimming or stretching may be safe, but high-impact activities should be avoided until symptoms settle.
Is hip bursitis a permanent condition?
No, hip bursitis is usually temporary and treatable. However, it may return if the underlying cause is not addressed.



