Piriformis
Syndrome
- Home
- Conditions We Treat
- Hip
- Piriformis Syndrome
What is piriformis syndrome?
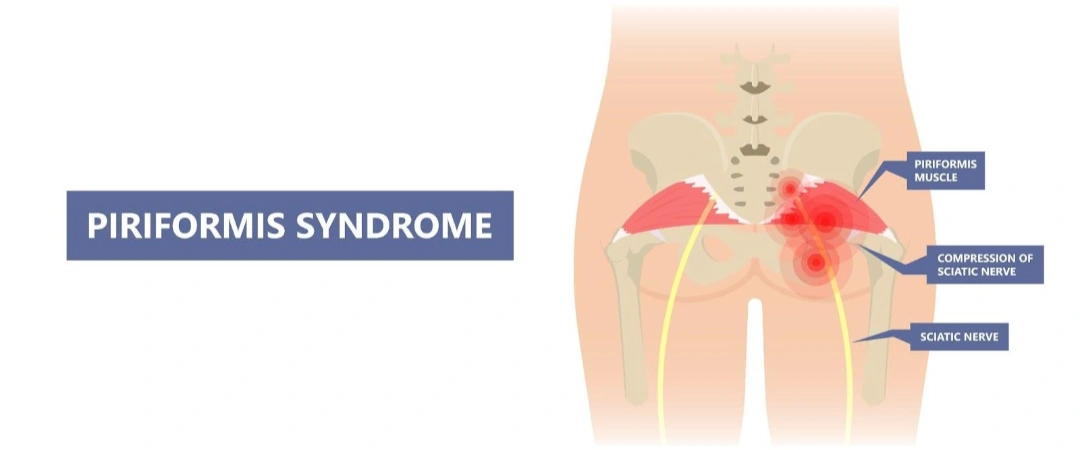
Piriformis syndrome is a neuromuscular condition in which the piriformis muscle, located deep within the buttock, behind the gluteus maximus, irritates or compresses the sciatic nerve. The piriformis muscle plays a crucial role in hip rotation, enabling the outward movement of the thigh. It lies in close proximity to the sciatic nerve, which is the largest nerve in the body and runs from the lower spine through the buttocks and down the legs.
In most individuals, the sciatic nerve passes beneath the piriformis muscle. However, anatomical variations exist, and in some people, the nerve may pass through or over the muscle, increasing the likelihood of compression. When the piriformis muscle becomes tight, inflamed, or spasmodic, often due to trauma, repetitive motion, prolonged sitting, or muscle imbalance, it can irritate the sciatic nerve. This results in symptoms such as buttock pain, leg numbness, tingling, or radiating discomfort down the thigh, mimicking sciatica.
Piriformis syndrome is considered a functional rather than structural cause of sciatic nerve irritation, which means that the symptoms arise from muscular dysfunction rather than disc herniation or spinal stenosis. As such, diagnosis can be challenging and often requires the exclusion of other spinal pathologies.

What causes piriformis syndrome?
Piriformis syndrome arises when the piriformis muscle compresses or irritates the sciatic nerve. This can be due to a range of functional or anatomical factors:
- Muscle overuse and strain — repetitive movements involving hip rotation, such as running, stair climbing, or prolonged cycling, can lead to overuse of the piriformis muscle. This may result in muscle tightness, inflammation, or spasm, increasing pressure on the sciatic nerve.
- Direct trauma to the buttock — a fall or blunt impact to the buttock region may cause local swelling, bruising, or scar tissue formation, all of which can irritate or entrap the sciatic nerve.
- Prolonged sitting or poor posture — spending long hours seated, particularly with inadequate support or pelvic misalignment, can cause the piriformis muscle to shorten or tighten, leading to nerve compression over time.
- Anatomical anomalies — in some individuals, the sciatic nerve passes through or above the piriformis muscle rather than beneath it. These structural variations can predispose the nerve to irritation with even minor muscle changes.
- Secondary causes — post-surgical scarring, pelvic instability, or masses near the sciatic nerve pathway may also contribute to piriformis syndrome, although these cases are less common.
The condition is often multifactorial, and recognising the contributing causes is key to devising an effective and targeted treatment plan.
What is the difference between piriformis syndrome versus sciatica?
While piriformis syndrome and sciatica share similar symptoms, such as buttock pain and radiating leg discomfort, they differ in terms of origin and underlying cause. Piriformis syndrome occurs when the piriformis muscle compresses or irritates the sciatic nerve as it passes through or beneath the muscle in the buttock. It is a non-spinal cause of sciatic nerve pain, typically associated with muscle tightness, trauma, repetitive strain, or anatomical variation.
In contrast, sciatica is a broader term referring to pain along the sciatic nerve pathway, most often resulting from spinal issues such as a herniated disc, spinal stenosis, or degenerative disc disease. In such cases, the compression originates in the lumbar spine rather than the buttock.
The table below lists the key differences between piriformis syndrome and sciatica.
| Feature | Piriformis Syndrome | Sciatica |
|---|---|---|
| Origin of pain | Buttock | Lower back |
| Cause of nerve compression | Compression by the piriformis muscle | Compression by spinal structures (e.g. herniated disc, spinal stenosis) |
| Type of condition | Muscular (extra-spinal) | Spinal |
| Common symptom pattern | Deep buttock pain, radiating down the back of the leg | Lower back pain radiating down the leg, often below the knee |
| Imaging findings | Usually normal (used to rule out spinal causes) | May show disc bulge, nerve root compression, or spinal narrowing |
| Aggravating factors | Sitting, climbing stairs, hip rotation | Bending, lifting, coughing, sitting |
| Physical exam findings | Pain on hip rotation or FAIR test | Positive straight leg raise test |
| Treatment focus | Stretching, physiotherapy, muscle release, injection therapy | Spinal therapy, anti-inflammatory medication, physiotherapy, in some cases surgery |
| Response to piriformis injection | Often relieves pain if correctly diagnosed | Typically no relief, as the issue is spinal |
What are the symptoms of piriformis syndrome?
Piriformis syndrome typically presents with symptoms related to irritation of the sciatic nerve, most often affecting one side of the body. The severity and nature of symptoms can vary depending on the degree of muscle tightness and nerve involvement.
- Buttock pain — a deep, aching discomfort is usually felt in the centre of the buttock, often described as sharp or burning during movement or prolonged sitting.
- Sciatica-like pain — pain may radiate from the buttock down the back of the thigh and sometimes into the lower leg, mimicking true sciatica caused by spinal disc issues.
- Numbness or tingling — some individuals report a pins-and-needles sensation, particularly in the buttock, back of the leg, or foot, indicating irritation of the sciatic nerve.
- Worsening with activity or sitting — symptoms often worsen with physical activities such as running, stair climbing, or squatting, as well as during prolonged periods of sitting or driving.
- Tenderness over the piriformis muscle — direct pressure over the buttock may reveal local tenderness, and in some cases, a palpable knot or tight band of muscle.
The symptoms of piriformis syndrome can overlap with other causes of sciatic nerve pain, which makes clinical evaluation important to differentiate it from spinal conditions such as a herniated disc or spinal stenosis.
Who is at risk of piriformis syndrome in Singapore?
Piriformis syndrome can affect individuals of all ages and activity levels, but certain factors may increase the likelihood of developing the condition.
- Athletes and physically active individuals — those who engage in sports involving repetitive hip and leg movements, such as runners, cyclists, and rowers, are at higher risk due to overuse and muscle strain.
- People with sedentary lifestyles — prolonged sitting, especially with poor posture or on hard surfaces, can cause the piriformis muscle to become tight or shortened, increasing the chance of nerve compression.
- Individuals with anatomical variations — people whose sciatic nerve passes through or over the piriformis muscle rather than beneath it may be more susceptible to compression and irritation.
- Those with previous trauma or injury — a direct injury to the buttock or pelvis, such as a fall or blunt force, may cause muscle inflammation or scarring, heightening the risk of piriformis syndrome.
- Women — the condition appears to be more common in women, possibly due to wider pelvic anatomy and hormonal factors that may affect muscle and ligament laxity.
How is piriformis syndrome diagnosed?
Diagnosing piriformis syndrome can be challenging, as its symptoms often mimic those of lumbar spine disorders. There is no single definitive test, so diagnosis is typically made through clinical evaluation and exclusion of other causes.
- Clinical history and symptom review — your doctor will begin by asking about the nature, duration, and pattern of your symptoms, particularly buttock pain and any radiation down the leg, to assess whether they are consistent with piriformis-related nerve irritation.
- Physical examination — specific movements and palpation may be used to reproduce symptoms. Tests such as the FAIR test (flexion, adduction, and internal rotation of the hip) may help identify pain caused by piriformis muscle tension or compression.
- Exclusion of spinal causes — imaging such as MRI or CT scans may be recommended to rule out other causes of sciatic nerve compression, including herniated discs, spinal stenosis, or tumours. These tests do not diagnose piriformis syndrome directly but are helpful in narrowing the possibilities.
- Electrodiagnostic studies — in some cases, electromyography (EMG) or nerve conduction studies may be performed to assess sciatic nerve function, though results may be normal in many cases of piriformis syndrome.
- Diagnostic injections — a local anaesthetic or corticosteroid injection into the piriformis muscle may be used both as a diagnostic tool and therapeutic option. Relief of symptoms following the injection supports the diagnosis.
A careful, stepwise approach is essential to confirm piriformis syndrome and ensure that treatment is appropriately targeted to the underlying cause of symptoms.
What are the treatment options for piriformis syndrome in Singapore?
Treatment for piriformis syndrome focuses on relieving muscle tension, reducing sciatic nerve irritation, and restoring normal movement. Most cases improve with non-surgical management, though persistent symptoms may require more targeted interventions.
- Activity modification and rest — temporarily avoiding activities that aggravate symptoms, such as running, prolonged sitting, or heavy lifting, can reduce inflammation and allow the muscle to heal.
- Stretching and physiotherapy — targeted stretching of the piriformis and surrounding hip muscles, guided by a physiotherapist, helps release tension and improve flexibility. Strengthening exercises for the core and pelvis may also correct muscle imbalances that contribute to the condition.
- Medications — non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may be prescribed to reduce pain and inflammation. Muscle relaxants or neuropathic pain medications may also be considered for more severe discomfort.
- Manual therapy — deep tissue massage, myofascial release, and trigger point therapy can help alleviate muscle tightness and improve blood flow in the affected area.
- Heat and cold therapy — applying ice packs can reduce inflammation in the acute phase, while heat therapy may help relax tight muscles and promote circulation during recovery.
- Injection therapy — corticosteroid or local anaesthetic injections into the piriformis muscle may provide relief for individuals with persistent pain. Botulinum toxin (Botox) injections may also be used in select cases to reduce muscle spasm.
- Surgical treatment — surgery is rarely needed, but in cases where conservative treatments fail and symptoms remain disabling, surgical release of the piriformis muscle or decompression of the sciatic nerve may be considered.
Treatment plans are typically personalised based on the severity and duration of symptoms, underlying causes, and patient activity levels. Early intervention and proper rehabilitation are key to preventing recurrence.
Summary
Piriformis syndrome is a neuromuscular condition in which the piriformis muscle irritates or compresses the sciatic nerve, leading to buttock pain and radiating leg discomfort that can mimic sciatica. It is most often caused by muscle overuse, trauma, prolonged sitting, or anatomical variations, and tends to affect athletes, sedentary individuals, and women more commonly.
If you are experiencing persistent buttock or leg pain suggestive of piriformis syndrome, schedule a consultation with Cove Orthopaedics for personalised evaluation and treatment.
Frequently asked questions
Can piriformis syndrome resolve on its own?
Yes, mild cases of piriformis syndrome can improve on their own with rest, stretching, and avoiding aggravating activities. However, persistent cases often require physiotherapy or other targeted treatments.
What is the usual recovery time for piriformis syndrome?
Recovery typically takes two to four weeks with consistent conservative treatment. In more chronic or severe cases, it may take several months for symptoms to fully resolve.
What is the prognosis for piriformis syndrome?
The long-term outlook for piriformis syndrome is generally positive. Most individuals recover fully with proper rehabilitation, posture correction, and exercise.
Are there self-care strategies to prevent piriformis syndrome from recurring?
Yes. Regular stretching, strengthening of core and hip muscles, proper posture, and avoiding prolonged sitting can reduce the risk of recurrence.
How can I sleep better with piriformis syndrome?
Sleeping on your back with a pillow under your knees or on your side with a pillow between your legs can help reduce pressure on the piriformis muscle and improve sleep comfort.
How can piriformis syndrome be distinguished from true sciatica without imaging?
Piriformis syndrome typically causes buttock pain that worsens with sitting or hip movement, while true sciatica often originates in the lower back and radiates below the knee.
Conditions We Treat








